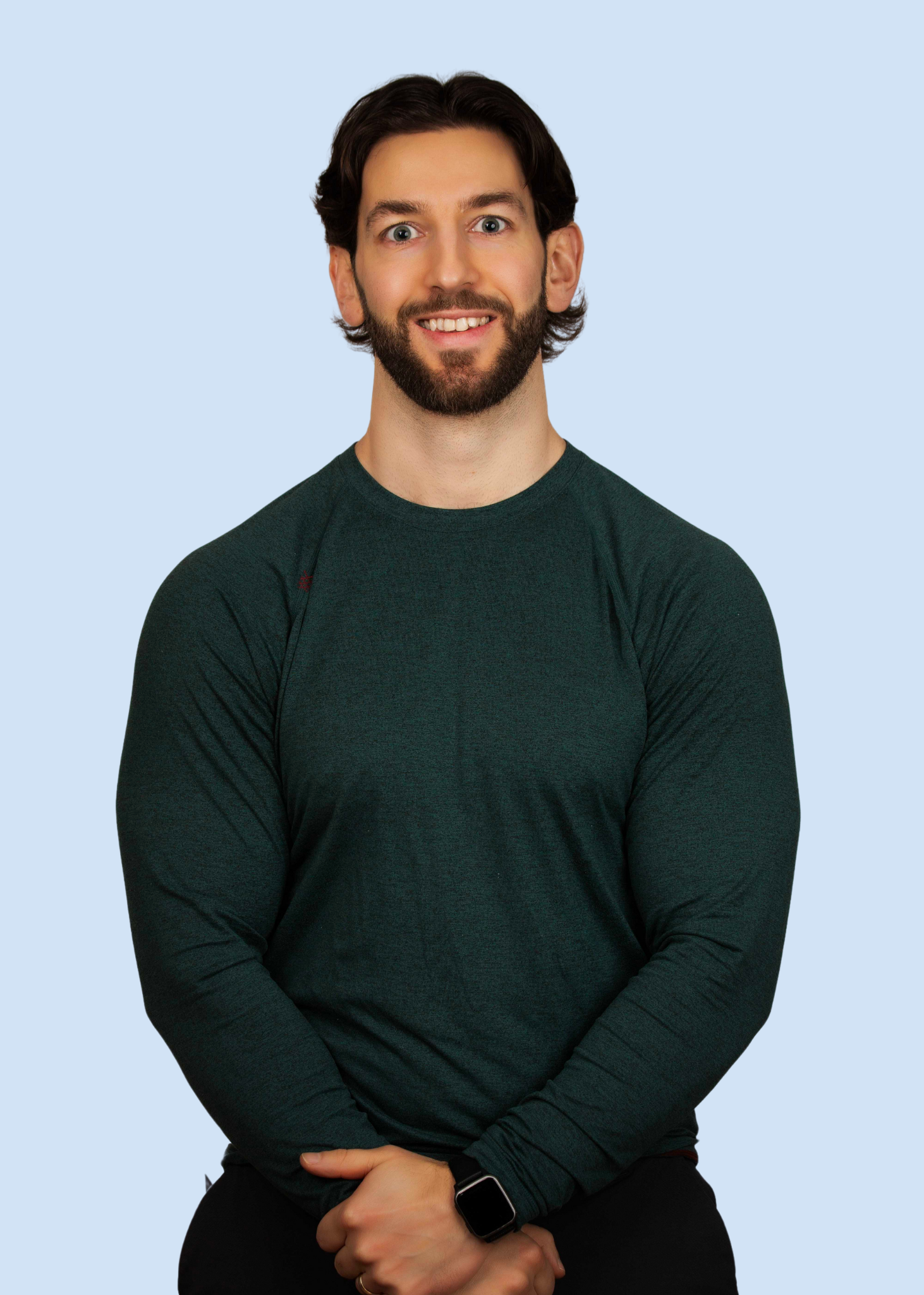
Your Partner in Pain-Free Living
I'm Jacob Perich, a passionate and dedicated physiotherapist committed to helping individuals overcome chronic pain and reclaim their lives. With years of experience and a deep understanding of the complexities of chronic pain management, I founded the Pacific Pain Centre with one goal in mind: to provide personalized care and effective treatment strategies to each of my clients.
My Journey
In September 2021, I embarked on a transformative journey following a series of three traumatic life events. Encountering debilitating pain accompanied by a myriad of perplexing symptoms, I sought answers from a variety of healthcare professionals over the course of three years, including doctors, neurologists, physiotherapists, massage therapists, naturopaths, pain specialists, psychologists, and counsellors. Despite receiving diverse diagnoses and conflicting treatment recommendations, my condition continued to deteriorate, leading to mounting frustrations and a deepening fear of movement and activity.
At my worst, I couldn’t walk for more than five minutes before the pain and numbness became unbearable. The activities that once brought me joy— running, hockey, lifting weights—were no longer options. Instead of excitement, they filled me with fear. Even the simplest daily tasks became a struggle, and just making it through the workday felt like an impossible challenge, day after day, for years. I couldn’t help but wonder, If this is me at 30, what does my future look like?
As my symptoms intensified, I shifted my perspective from associating symptom escalation with a worsening physical condition to understanding the role of sensitized tissue and a dysregulated nervous system in amplifying my pain experience. Embracing insights from Pain Reprocessing Therapy, pain neuroscience education, and mind-body medicine, I began to explore techniques aimed at regulating my nervous system and managing my chronic pain. This pivotal shift marked a turning point in my journey, offering newfound hope and empowerment in navigating the complexities of chronic pain management.
-
Lower back pain
Mid back pain
Neck pain
Left Anterior hip pain
Right posterior hip pain
Hamstring nerve tension
Quads nerve tension
Right knee pain
Left achilles pain
Right Shoulder pain
Right elbow pain
Left Leg numbness
Right foot numbness
Full body fasciculations/twitching
Hives/rashes
Skin mottling
Abdominal pain and
IBS
Headache
Fatigue
Blurred vision
Eye floaters
Frequently Sick
Conditions we treat
-
Nociplastic pain is a type of pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors, or evidence for disease or lesion of the somatosensory system causing the pain.
-
Neuroplastic pain refers to pain that arises from changes in the nervous system not due to physical injury or damage, but rather from the brain's ability to reorganize itself. This type of pain is often a result of neural pathways becoming sensitized or altered due to factors such as stress, trauma, or prolonged pain experiences. Unlike traditional pain that has a clear physical cause, neuroplastic pain is more about how the brain interprets and processes pain signals. Treatment often involves approaches like cognitive behavioral therapy, mindfulness, and other techniques aimed at retraining the brain and reducing the perceived pain.
-
Psychosomatic pain refers to physical pain that is influenced or exacerbated by psychological factors such as stress, anxiety, or depression. While the pain is real, its origin or intensity is linked to the mind-body connection rather than a purely physical cause. This type of pain can manifest in various forms, such as headaches, back pain, or stomach issues, and often requires a holistic approach to treatment, addressing both the physical symptoms and the underlying psychological factors.
-
Tension Myositis Syndrome (TMS), also known as Tension Myoneural Syndrome, is a term coined by Dr. John E.Sarno. It describes a psychosomatic condition where emotional stress and tension lead to physical symptoms, particularly chronic pain. Dr. Sarno believed that the brain distracts an individual from emotional issues by creating pain in the body, often in the back, neck, or limbs. The theory suggests that addressing the underlying emotional issues can alleviate the physical symptoms.
-
Mind-body pain refers to physical discomfort that is influenced by psychological factors. This type of pain often stems from stress, anxiety, depression, or emotional distress. The mind and body are interconnected, meaning mental states can manifest as physical symptoms.
Providing Services for
I support people living with ongoing or chronic pain—whether it's back pain, nerve pain, joint pain, fibromyalgia, or pain that hasn't had a clear diagnosis. If you're feeling stuck, frustrated, or unheard, you're not alone. I’m here to walk alongside you with a gentle, science-based approach that helps you make sense of your pain, reconnect with your body, and move toward the life you want to live—one step at a time
-
What it is
Chronic spinal pain refers to back or neck discomfort lasting longer than 3 months, often without a clear ongoing injury. It can develop after an accident, from long-term tension, or seemingly out of nowhere.
Prevalence & Key Stats
Up to 20% of adults experience chronic back or neck pain at any given time (Clark & Horton, 2018)
Disc bulges and degeneration are found in over 80% of people without any symptoms (Brinjikji et al., 2015)
In most cases, pain persists without clear structural damage or ongoing inflammation (Maher et al., 2017)
Over 90% of back pain is non-specific, meaning it can’t be traced to a single anatomical cause (Koes et al., 2006)
Why a Nervous System Approach Helps
Chronic spinal pain is often maintained by a sensitized nervous system, where the brain and spinal cord become overprotective and amplify danger signals (Apkarian et al., 2009). Even after tissues have healed, the system may stay hypervigilant. A nervous system-based approach focuses on calming this overactivity through education, nervous system regulation, and graded exposure—helping reduce pain and restore movement without relying on scans, injections, or surgery (Nijs et al., 2010).
-
What it is
Fibromyalgia is a long-term pain condition characterized by widespread body pain, fatigue, sleep issues, and cognitive difficulties ("fibro fog"). It’s not caused by tissue damage or inflammation, but by changes in how the brain and nervous system process pain signals.
Prevalence & Key Stats
Affects approximately 2–4% of the population, more common in women (Queiroz, 2013)
Diagnosis is often delayed or missed; symptoms overlap with many other conditions
Brain imaging studies show increased pain processing activity in response to normal input (Schweinhardt et al., 2008)
Up to 80–90% of people with fibromyalgia show signs of central sensitization (Clauw, 2015)
Why a Nervous System Approach Helps
Fibromyalgia is considered a classic example of central sensitization, when the nervous system becomes hypersensitive and pain signals are amplified (Yunus, 2007). Since the pain is not due to ongoing tissue damage, treatments aimed at calming and retraining the nervous system, such as pain neuroscience education, gentle movement, nervous system regulation, and cognitive strategies, can be highly effective at reducing symptoms and restoring quality of life (Nijs et al., 2011).
-
What it is
Myofascial Pain Syndrome (MPS) involves pain and tenderness in specific muscles or regions of the body, often linked to sensitive "trigger points" in the muscle or fascia. These points can cause referred pain, stiffness, and local twitch responses. Unlike a temporary muscle strain, MPS tends to persist over time and may not respond to stretching or massage alone.
Prevalence & Key Stats
Estimated to affect 30–85% of patients in chronic pain clinics (Gerwin et al., 2004)
Trigger points are common, but not always painful; they are also found in people without symptoms (Lucas et al., 2009)
Muscle pain without injury may stem more from nervous system changes than local tissue damage
MPS frequently overlaps with other central sensitization conditions like fibromyalgia, tension headaches, and IBS (Giamberardino et al., 2011)
Why a Nervous System Approach Helps
While trigger points are located in muscles, their sensitivity is often maintained by a sensitized nervous system, not just local tissue dysfunction. Central sensitization can cause even normal muscle activity or touch to be perceived as painful. Addressing this through nervous system education, desensitization strategies, stress reduction, and movement retraining helps reduce both the local and widespread pain associated with MPS (Shah & Gilliams, 2008; Nijs et al., 2010).
-
What it is
Chronic headaches, including tension-type headaches, migraines, and cervicogenic headaches can cause persistent pain in the head, temples, jaw, or neck. These are not usually caused by structural problems in the brain, but rather by complex interactions between the nervous system, muscles, and stress systems.
Prevalence & Key Stats
Headaches are one of the most common pain complaints globally, with up to 46% of adults experiencing active headache disorders (Stovner et al., 2007)
Tension-type headaches are the most common form, affecting roughly 20–30% of the population (Jensen & Stovner, 2008)
Brain imaging is typically normal and not routinely needed for most headache types
Headaches often co-occur with other signs of nervous system sensitization such as fibromyalgia, jaw pain, and irritable bowel syndrome (Simons et al., 1999; Fernández-de-las-Peñas et al., 2007)
Why a Nervous System Approach Helps
Chronic headaches are frequently linked to an overactive or sensitized nervous system, where pain pathways become hypersensitive and trigger headaches from minor inputs like stress, posture, or muscle tension. Education, nervous system regulation, and desensitization techniques, including stress reduction, gentle movement, and pain retraining, can help reduce the frequency and intensity of headaches without relying solely on medication (Nijs et al., 2014; Coppieters et al., 2021).
-
What it is
IBS is a common functional gut disorder involving recurring abdominal pain, bloating, gas, and changes in bowel habits (diarrhea, constipation, or both). It is not caused by inflammation or structural disease, but by altered communication between the gut and the brain.
Prevalence & Key Stats
Affects approximately 10–15% of the global population (Lovell & Ford, 2012)
Symptoms often flare with stress, food intolerance, or hormonal shifts
Standard imaging and lab tests are typically normal or inconclusive
IBS is highly comorbid with other central sensitivity syndromes such as fibromyalgia and chronic fatigue syndrome (Yunus, 2007)
Functional MRI studies show enhanced pain processing in brain regions linked to emotion and visceral sensation in IBS patients (Mayer et al., 2015)
Why a Nervous System Approach Helps
IBS is increasingly understood as a disorder of the gut-brain axis, where the nervous system misinterprets normal digestive signals as threats. Chronic stress, early life adversity, and sensitization of the enteric nervous system can heighten visceral pain sensitivity. A neuroplastic approach addressing fear, nervous system regulation, interoceptive awareness, and gut-directed cognitive or somatic strategies, can significantly reduce IBS symptoms without relying solely on restrictive diets or medication (Moseley et al., 2021; Lackner et al., 2018).
-
What it is
CRPS is a chronic pain condition that usually develops after an injury, surgery, or fracture, most commonly in the arm or leg. It involves severe, ongoing pain along with changes in skin color, temperature, swelling, and motor function. The pain is often out of proportion to the original injury.
Prevalence & Key Stats
CRPS affects an estimated 5.5–26.2 people per 100,000 annually (de Mos et al., 2007)
It is more common in women and typically begins between the ages of 40 and 60
Symptoms can persist long after the tissue has healed and may spread beyond the original injury site
Studies show abnormal pain processing in the brain, including changes in somatosensory and motor cortical maps (Maihöfner et al., 2003)
Why a Nervous System Approach Helps
CRPS is considered one of the most clear examples of central sensitization and altered brain-body communication. The nervous system becomes stuck in a state of heightened protection, amplifying pain, swelling, and sensitivity. A neuroplastic approach using graded motor imagery, pain neuroscience education, mirror therapy, and nervous system regulation, can help retrain the brain, reduce hypersensitivity, and restore movement and function over time (Moseley, 2006; Birklein & Schlereth, 2015).
-
What it is
Phantom limb pain refers to pain sensations that are felt in a limb or body part that has been amputated. The pain can feel sharp, burning, cramping, or electric-like, and often occurs even though the limb is no longer present. This is different from residual limb (stump) pain, which occurs in the remaining tissue.
Prevalence & Key Stats
Affects up to 80% of amputees, often beginning within days or weeks of surgery (Kooijman et al., 2000)
The intensity and frequency vary widely, and the pain can persist for years
Brain imaging shows reorganization in the somatosensory cortex—areas that once represented the lost limb become taken over by neighboring areas (Flor et al., 2006)
Emotional distress, pre-amputation pain, and lack of movement strategies increase risk of persistent symptoms (Wartan et al., 1997)
Why a Nervous System Approach Helps
Phantom limb pain is a prime example of pain generated by the brain and nervous system rather than by tissue damage. After amputation, the brain continues to "expect" input from the missing limb, and the nervous system may amplify signals as a protective response. A neuroplastic approach—using graded motor imagery, mirror therapy, pain education, and nervous system regulation, can help remap the brain, reduce fear, and decrease pain intensity by calming and retraining the system (Moseley, 2007; Chan et al., 2007).
-
What it is
TMJ Disorder refers to pain and dysfunction in the jaw joint and surrounding muscles. It may involve clicking, locking, difficulty opening the mouth, or pain that radiates into the face, neck, or head. While it can begin after dental work, injury, or teeth grinding, many cases develop without a clear cause.
Prevalence & Key Stats
TMD affects approximately 5–12% of the population, more commonly in women (Slade et al., 2016)
In most cases, imaging of the joint shows no serious structural damage
Symptoms often overlap with tension headaches, neck pain, and fibromyalgia—suggesting a shared underlying mechanism (Häggman-Henrikson et al., 2020)
Over 40% of people with TMD show signs of central sensitization or nervous system amplification (Wright et al., 2010)
Why a Nervous System Approach Helps
Chronic TMJ pain often persists long after the original tissue irritation has resolved. In these cases, the nervous system becomes sensitized, responding more strongly to minor jaw movements, touch, or even stress. A neuroplastic approach helps by calming this sensitization through pain education, nervous system regulation, and gentle jaw and neck desensitization strategies. This improves comfort, jaw function, and reduces fear and tension that often maintain the cycle of pain (Nijs et al., 2010; Leeuw et al., 2009).
-
What it is
Chronic pelvic pain (CPP) refers to pain in the lower abdomen, pelvis, hips, or pelvic floor that lasts longer than 3–6 months. It may be associated with menstruation, urination, bowel movements, or sexual activity, or persist independently of any specific activity. CPP can occur with or without identifiable pathology in the muscles, joints, or organs.
Prevalence & Key Stats
Affects up to 15–20% of women and a growing number of men (Mathias et al., 1996; Clemens et al., 2007)
In more than 50% of cases, no ongoing structural cause is found (Reiter, 1990)
Many patients are diagnosed with overlapping conditions such as endometriosis, interstitial cystitis, IBS, or pudendal neuralgia
Central sensitization is present in a large subset of chronic pelvic pain patients, contributing to widespread pain and symptom amplification (Fitzgerald et al., 2019)
Why a Nervous System Approach Helps
Even when the original cause of pelvic pain has resolved, or no clear source is found, the nervous system may stay in a sensitized, hyper-protective state. This can lead to increased pain sensitivity, guarding, muscle tension, and fear of movement or intimacy. A neuroplastic approach helps calm this heightened reactivity through nervous system regulation, pain neuroscience education, gentle movement, and pelvic-focused desensitization techniques. This whole-person model supports physical and emotional recovery where other approaches may have fallen short (Nijs et al., 2014; Engeler et al., 2019).
-
What it is
Chronic Fatigue Syndrome, or Myalgic Encephalomyelitis (ME/CFS), is a complex condition marked by profound fatigue that isn’t relieved by rest, along with brain fog, unrefreshing sleep, dizziness, and a worsening of symptoms after exertion (known as post-exertional malaise). It is not explained by other medical or psychiatric conditions and can severely impact quality of life.
Prevalence & Key Stats
Affects an estimated 0.4–1% of the population worldwide (Johnston et al., 2013)
Post-exertional symptom worsening is reported in over 90% of ME/CFS patients (Chu et al., 2018)
Brain imaging and autonomic testing show nervous system dysregulation and impaired energy metabolism (Barnden et al., 2011; VanElzakker, 2013)
Up to 80% of people with ME/CFS show signs of central sensitization or heightened pain and fatigue processing (Meeus et al., 2013)
Why a Nervous System Approach Helps
ME/CFS is increasingly understood as a condition involving nervous system dysregulation, particularly in how the brain processes fatigue, stress, pain, and internal body signals (interoception). Many patients remain stuck in a cycle of energy crashes, fear of exertion, and nervous system hypervigilance. A neuroplastic approach, focused on pacing, interoceptive awareness, graded nervous system regulation, and desensitization can help reduce symptom flares and rebuild a foundation for recovery without pushing through or ignoring the body’s signals (Nijs et al., 2008; Jason et al., 2021).
-
What it is
Peripheral neuropathy refers to damage or dysfunction of the peripheral nerves, which carry messages between the brain/spinal cord and the rest of the body. It can cause symptoms like burning, tingling, numbness, hypersensitivity, or weakness, often starting in the hands or feet. It may result from diabetes, injury, infections, chemotherapy, or have no clear cause.
Prevalence & Key Stats
Affects up to 7–10% of the general population, and over 50% of people with diabetes (Callaghan et al., 2015; Feldman et al., 2019)
Many patients continue to experience symptoms even after the underlying cause is treated or stabilized
In some cases, symptoms persist despite no ongoing nerve damage being seen on EMG or imaging (Bouhassira et al., 2005)
Central sensitization and altered brain processing contribute to pain in many cases of chronic neuropathy (Baron et al., 2010)
Why a Nervous System Approach Helps
While peripheral nerve damage may have started the process, the ongoing pain in many neuropathy cases is maintained by changes in the central nervous system. This includes heightened sensitivity to stimuli (e.g. light touch or temperature) and brain-based amplification of pain signals. A neuroplastic approach helps calm and retrain the nervous system using education, sensory re-integration, graded desensitization, and regulation techniques, offering relief even when medications or nerve-focused treatments have failed (Moseley & Flor, 2012; Nijs et al., 2010).
-
What it is
Trigeminal neuralgia is a chronic facial pain condition affecting the trigeminal nerve, which carries sensation from the face to the brain. It causes sudden, severe, electric shock-like pain in the jaw, cheek, or around the eye, often triggered by touch, talking, chewing, or brushing teeth. Pain episodes can last seconds to minutes and may occur repeatedly throughout the day.
Prevalence & Key Stats
Affects approximately 4–13 people per 100,000 annually, most commonly in adults over 50 and more often in women (Maarbjerg et al., 2017)
Most cases are classified as "idiopathic," meaning no structural compression or lesion is found
Even when nerve compression is present, pain often persists despite surgery or medication (Zakrzewska & Linskey, 2014)
Studies show altered brain processing and sensory integration in chronic cases, suggesting involvement of central sensitization (Moisset et al., 2011)
Why a Nervous System Approach Helps
While trigeminal neuralgia often begins with irritation of the trigeminal nerve, ongoing pain may be maintained by changes in the brain and spinal cord that amplify pain signals. In these cases, the nervous system becomes overly sensitive, even to light touch or emotion. A neuroplastic approach helps calm this sensitivity by targeting fear, threat perception, and pain pathways through education, somatosensory retraining, and nervous system regulation. This offers a promising path forward, especially for those who have not responded well to medication or surgery (Nijs et al., 2010; Moisset & Bouhassira, 2007).
-
What it is
Chronic whiplash syndrome refers to ongoing neck pain, stiffness, headaches, dizziness, and fatigue that persist for months after a whiplash injury, typically caused by a motor vehicle accident or sudden impact. While acute symptoms usually resolve within weeks, some individuals experience prolonged pain and disability despite no evidence of serious tissue damage.
Prevalence & Key Stats
Up to 50% of people with whiplash injuries report persistent symptoms 12 months after the incident (Carroll et al., 2008)
Imaging (MRI, X-ray) rarely shows significant structural damage in chronic whiplash cases (Pettersson et al., 1997)
High rates of central sensitization, fear of movement, and altered pain processing are found in those with chronic symptoms (Sterling et al., 2003)
Symptoms often extend beyond the neck, including widespread sensitivity, fatigue, and cognitive complaints
Why a Nervous System Approach Helps
In chronic whiplash, the original injury may have healed, but the nervous system can remain stuck in a state of heightened protection, amplifying pain and tension signals. This is known as central sensitization. A neuroplastic approach helps calm and retrain the system through pain neuroscience education, graded exposure, stress regulation, and gentle movement strategies. This approach helps patients reduce symptoms, regain trust in their bodies, and recover function even when pain has been persistent (Nijs et al., 2010; Coppieters et al., 2020).
-
What it is
Post-surgical pain is expected in the short term after surgery, but for some people, pain persists for months or even years after the procedure. This is referred to as persistent post-surgical pain (PPSP) and is not always linked to complications or tissue damage. The pain may be sharp, burning, aching, or nerve-like, and can significantly impact function and recovery.
Prevalence & Key Stats
Persistent post-surgical pain affects 10–50% of patients depending on the surgery type (Kehlet et al., 2006)
High-risk surgeries include mastectomy, hernia repair, thoracotomy, and joint replacement
In many cases, imaging and healing appear normal, but the pain remains (Katz & Seltzer, 2009)
Central sensitization, fear, and stress are key contributors to the transition from acute to chronic pain after surgery (Lavand'homme, 2017)
Why a Nervous System Approach Helps
When pain lasts beyond normal healing time, the nervous system may be stuck in “protection mode.” The brain and spinal cord continue to amplify signals even in the absence of tissue damage, a process known as central sensitization. Our approach focuses on calming the nervous system through education, gentle movement, desensitization, and emotional processing. This helps retrain pain pathways and restore function, even months or years after surgery (Nijs et al., 2014; Clarke et al., 2012).
-
What it is
Osteoarthritis (OA) is a common joint condition involving the gradual breakdown of cartilage, often leading to joint stiffness, swelling, and pain especially in the knees, hips, hands, and spine. While structural changes are visible on X-rays or MRIs, pain levels often do not match the degree of joint degeneration.
Prevalence & Key Stats
Affects over 300 million people worldwide and is the leading cause of disability in older adults (Hunter & Bierma-Zeinstra, 2019)
Up to 40% of people with moderate to severe joint degeneration on imaging report little to no pain (Bedson & Croft, 2008)
Conversely, many people with joint pain show only mild or no visible joint changes
Central sensitization and fear of movement are common in individuals with chronic OA pain (Lluch et al., 2014)
Why a Nervous System Approach Helps
While joint changes are part of normal aging, chronic OA pain is often amplified by the nervous system, especially when pain persists beyond what would be expected from the degree of wear and tear. Central sensitization can cause the brain to interpret normal movement as threatening. Our approach helps reduce this amplification through pain education, movement confidence building, desensitization, and nervous system regulation. This empowers people with OA to move more freely and manage symptoms without relying solely on injections or surgery (Nijs et al., 2014; Farrell et al., 2019).
-
What it is
Psoriatic arthritis is an inflammatory autoimmune condition that affects both the skin and joints. It commonly causes joint pain, stiffness, swelling, and fatigue, often alongside skin plaques from psoriasis. PsA can affect any joint, including the spine (axial PsA), and may also cause enthesitis (pain where tendons attach to bone) or dactylitis (sausage digits).
Prevalence & Key Stats
Affects up to 30% of people with psoriasis, typically developing between ages 30–50 (Ogdie & Weiss, 2015)
Pain and fatigue often persist even when inflammation is controlled with medication
Central sensitization is present in up to 50% of PsA patients, amplifying pain and disability (Mease et al., 2020)
Up to 20% of individuals with PsA meet criteria for fibromyalgia, making pain more widespread and less inflammation-dependent (Orbai et al., 2014)
Why a Nervous System Approach Helps
While PsA involves real immune-driven inflammation, many people continue to experience chronic pain due to a sensitized nervous system. This leads to heightened pain perception and a mismatch between imaging/lab results and how the body feels. Our approach works alongside medical treatment to help reduce nervous system amplification through pain education, movement retraining, and stress regulation, supporting improved function and quality of life even in the presence of an autoimmune condition (Nijs et al., 2010; Mease et al., 2020).
-
What it is
Ankylosing spondylitis is a type of inflammatory arthritis that primarily affects the spine and sacroiliac joints, leading to stiffness, pain, and reduced mobility. It is a chronic autoimmune condition that can also involve the hips, shoulders, eyes (uveitis), and tendons. Over time, the spine may fuse or become less flexible.
Prevalence & Key Stats
Affects about 0.1–1.4% of the population, typically beginning before age 40 and more common in males (Dean et al., 2014)
The average delay in diagnosis is 5–10 years due to misattribution of symptoms to mechanical back pain (Rudwaleit et al., 2004)
Many individuals report widespread pain, fatigue, and psychological distress, even when inflammation is controlled
Up to 30–50% of AS patients show signs of central sensitization and pain amplification beyond spinal inflammation (de Koning et al., 2018)
Why a Nervous System Approach Helps
While AS is an inflammatory disease, many people experience ongoing pain, fatigue, and flares due in part to nervous system sensitization, where the brain remains on high alert and amplifies signals even after inflammation subsides. Our approach complements medical treatment by addressing this neuroplastic pain through education, gentle movement, pain desensitization, and nervous system regulation, helping reduce flare-ups, improve function, and restore confidence in the body (Nijs et al., 2014; de Koning et al., 2018).
-
What it is
Axial spondyloarthritis (axSpA) is a type of inflammatory arthritis that mainly affects the spine, pelvis, and sacroiliac joints. It includes both ankylosing spondylitis (where changes appear on X-ray) and non-radiographic axSpA (where symptoms are present but X-rays are normal). People with axSpA often experience deep spinal stiffness, fatigue, and flares of inflammatory pain, especially in the morning or after rest.
Prevalence & Key Stats
Affects approximately 0.5–1.4% of the population globally, often beginning before age 45 (Deodhar et al., 2014)
Women are more likely to be diagnosed with non-radiographic axSpA and may have fewer visible changes on imaging
Diagnostic delays average 5–8 years due to overlap with mechanical back pain and normal early imaging (Rudwaleit et al., 2009)
Central sensitization affects up to 50% of individuals with axSpA and contributes to persistent pain and fatigue even when inflammation is under control (de Koning et al., 2018)
Why a Nervous System Approach Helps
While axSpA involves real inflammatory changes, research shows that ongoing pain is often worsened by nervous system sensitization, where the brain and spinal cord remain in a hypervigilant state. This can amplify pain even after inflammation subsides or when scans appear normal. Our approach complements medical care by helping calm the nervous system through pain education, movement desensitization, pacing strategies, and stress regulation, offering relief beyond what medications alone can achieve (Nijs et al., 2014; de Koning et al., 2018).
-
What it is
Chronic tendinitis, now more accurately referred to as tendinopathy, involves persistent pain and dysfunction in a tendon (such as the Achilles, rotator cuff, patellar, or elbow tendons). It’s often described as an "overuse injury," but long-term tendon pain typically occurs without signs of active inflammation or tissue tearing. It may linger for months despite rest, exercise, or even imaging that appears normal.
Prevalence & Key Stats
Tendinopathy accounts for up to 30–50% of all sports-related injuries (Albers et al., 2020)
Chronic tendon pain can persist even after the tendon has structurally adapted or imaging findings have improved
Studies show a poor correlation between tendon pathology on imaging and pain severity (Cook & Purdam, 2009)
Central sensitization is present in a significant portion of chronic tendinopathy cases, especially when pain is widespread or unresponsive to loading programs (Plinsinga et al., 2015)
Why a Nervous System Approach Helps
In persistent tendinopathy, the pain may no longer be caused by damage to the tendon, but rather by a sensitized nervous system that continues to protect the area. This heightened sensitivity can amplify pain during loading or movement, even when the tendon is safe to use. Our approach helps calm the system and restore confidence in movement through pain education, graded exposure, nervous system regulation, and reconceptualizing the pain experience. This supports tissue recovery while addressing the deeper nervous system drivers (Nijs et al., 2014; Rio et al., 2016).
-
What it is
Bursitis refers to inflammation or irritation of a bursa, a small fluid-filled sac that cushions joints and tendons. Common sites include the shoulder, hip, elbow, and knee. While acute bursitis may result from trauma or repetitive strain, chronic bursitis involves persistent pain that continues long after the initial flare or injury has resolved, often without ongoing inflammation.
Prevalence & Key Stats
Subacromial (shoulder) bursitis is one of the most common causes of shoulder pain, with prevalence estimates ranging from 20–50% in adults with shoulder complaints (Luime et al., 2004)
Hip (trochanteric) bursitis affects up to 15% of women and 8% of men over age 50 (Segal et al., 2007)
Chronic bursitis often shows no signs of active inflammation on imaging, despite ongoing pain
Central sensitization and nervous system hyperexcitability may explain persistent pain when imaging and lab markers are normal (Plinsinga et al., 2015)
Why a Nervous System Approach Helps
In chronic bursitis, pain may no longer reflect tissue inflammation but rather a sensitized nervous system that continues to “protect” the area long after healing. This can make movement feel threatening or painful, even when the joint is safe to use. Our approach focuses on reducing this nervous system overactivity using pain neuroscience education, desensitization, graded movement, and nervous system regulation, helping to restore confidence and reduce pain without relying solely on injections or anti-inflammatory treatments (Nijs et al., 2014; Rio et al., 2016).
-
What it is
Plantar fasciitis refers to pain at the bottom of the heel, often worst with the first steps in the morning or after rest. While traditionally considered an “inflammatory” condition, research shows that in chronic cases, there is little to no inflammation, making fasciosis (degeneration and sensitivity of the fascia) a more accurate term. The pain often persists long after the tissue should have healed.
Prevalence & Key Stats
Affects up to 10% of the population at some point, and is one of the most common causes of heel pain (Riddle et al., 2004)
In many cases, symptoms last longer than 6–12 months despite conservative care
Imaging (e.g. ultrasound, MRI) may show thickening of the fascia—but the severity of pain doesn’t always match structural findings (Gibbon & Long, 1999)
Many individuals with chronic plantar fasciitis show signs of central sensitization, particularly when pain spreads or becomes unpredictable (Plinsinga et al., 2015)
Why a Nervous System Approach Helps
When heel pain continues long after the initial injury or overload, it may no longer be driven by tissue damage, but by a sensitized nervous system. The brain may continue to interpret walking or standing as threatening, leading to amplified pain signals. Our approach helps retrain this system through pain education, desensitization, graded loading, and nervous system regulation, offering a way forward for people whose pain has become persistent or resistant to standard treatment (Nijs et al., 2014; Rio et al., 2016).
-
What it is
Carpal Tunnel Syndrome is a condition where the median nerve becomes irritated or compressed as it passes through the carpal tunnel in the wrist. It often causes numbness, tingling, weakness, or pain in the thumb, index, and middle fingers. While many cases are mild and resolve with rest or activity modification, others persist or recur despite treatment, even when nerve tests or scans are normal.
Prevalence & Key Stats
Affects approximately 3–6% of adults, more common in women and people doing repetitive hand tasks (Atroshi et al., 1999)
Up to 35% of people diagnosed with CTS continue to have symptoms after surgery (Jerosch-Herold et al., 2017)
Nerve conduction studies may be normal in up to 18% of patients with CTS-like symptoms (Mondelli et al., 2004)
Central sensitization and cortical reorganization have been identified in persistent CTS cases, even after decompression (Barbieri et al., 2020)
Why a Nervous System Approach Helps
When CTS symptoms linger or return after healing or surgery, a sensitized nervous system may be keeping the area in “protection mode,” amplifying normal signals as painful or threatening. This is especially likely when symptoms are widespread, inconsistent, or associated with high stress or fear. Our approach helps by calming the nervous system through education, sensory retraining, nervous system regulation, and graded movement strategies, supporting long-term recovery, even in complex or persistent cases (Nijs et al., 2014; Coppieters & Butler, 2008).
-
What it is
Cubital Tunnel Syndrome is a condition where the ulnar nerve becomes compressed or irritated as it passes behind the elbow (the “funny bone” area). It can cause numbness, tingling, weakness, or pain in the ring and little fingers, often worse when the elbow is bent for long periods (e.g. sleeping, driving, or using a phone).
Prevalence & Key Stats
Second most common peripheral nerve entrapment after carpal tunnel syndrome (Mowlavi et al., 2000)
Affects approximately 1–3% of the general population, more common in people who lean on their elbows frequently or have repetitive arm movements
Up to 50% of people continue to experience symptoms after surgical decompression, even when nerve conduction improves (Bartels et al., 2005)
Studies show altered central nervous system processing and cortical changes in chronic cases, indicating central sensitization (Schmid et al., 2014)
Why a Nervous System Approach Helps
When symptoms persist after rest, splinting, or even surgery, it may be due to nervous system sensitization, where the brain continues to amplify signals and protect the area long after tissue healing. This can lead to heightened sensitivity, unpredictable pain, and movement fear. Our approach targets the nervous system directly through pain education, sensory retraining, neural mobilization, and regulation strategies to reduce symptoms and restore confidence in arm use, even in complex or post-surgical cases (Nijs et al., 2014; Coppieters & Butler, 2008).
-
What it is
Tarsal Tunnel Syndrome (TTS) is a condition where the posterior tibial nerve is compressed or irritated as it passes through the tarsal tunnel on the inside of the ankle. This can cause burning, tingling, numbness, or sharp pain in the heel, arch, sole, or toes. Symptoms often worsen with standing, walking, or at night, and may mimic plantar fasciitis or peripheral neuropathy.
Prevalence & Key Stats
Considered less common than carpal or cubital tunnel syndrome, with exact prevalence unknown but often underdiagnosed
Frequently misdiagnosed as plantar fasciitis due to overlapping symptoms (Barker et al., 2007)
Imaging and nerve conduction studies may be inconclusive, especially in early or intermittent cases
Persistent cases often involve central sensitization, where pain remains despite minimal nerve compression or after surgical decompression (Kinoshita et al., 2015)
Why a Nervous System Approach Helps
When tarsal tunnel symptoms continue despite rest, orthotics, or surgery, the pain may be driven more by a sensitized nervous system than by ongoing compression. The brain can become overprotective, amplifying pain and causing symptoms to persist even when tissue stress is low. Our approach targets this sensitization using pain education, graded movement, neural mobilization, and nervous system regulation strategies, helping to reduce symptoms and restore mobility over time (Nijs et al., 2014; Coppieters & Butler, 2008).
-
What it is
Thoracic Outlet Syndrome refers to a group of conditions where nerves and/or blood vessels are compressed or irritated as they pass through the thoracic outlet, the space between the collarbone and first rib. It can cause pain, numbness, tingling, or weakness in the neck, shoulder, arm, or hand. Symptoms may worsen with posture, repetitive movements, or carrying objects.
Prevalence & Key Stats
Affects approximately 3–8 out of 100,000 people annually, but likely underdiagnosed (Sanders et al., 2007)
Over 90% of cases are neurogenic TOS, where symptoms stem from nerve irritation without major vascular involvement (Ferrante, 2012)
Many individuals show no clear structural cause on imaging, and nerve conduction tests may be normal
Central sensitization is often involved in chronic TOS, especially when symptoms spread, fluctuate, or persist despite tissue-based treatments (Schmid et al., 2014)
Why a Nervous System Approach Helps
In chronic or non-specific TOS, the nervous system may become hypersensitive, continuing to interpret normal postures or movements as threatening, even after any initial compression has resolved. This leads to ongoing pain, tightness, or weakness that doesn’t respond well to standard physical therapy or surgery. Our approach focuses on calming the nervous system using pain education, graded movement, postural retraining, neural mobilization, and stress regulation, helping restore function and reduce symptoms without relying solely on structural correction (Nijs et al., 2014; Coppieters & Butler, 2008).
-
What it is
Meralgia paresthetica is a condition caused by irritation or compression of the lateral femoral cutaneous nerve, which supplies sensation to the outer thigh. It often leads to burning, tingling, numbness, or sensitivity in the upper outer thigh. The pain is usually surface-level (not deep in the muscles or joints) and is not caused by injury or damage to the leg muscles or spine.
Prevalence & Key Stats
Estimated to affect 4–7 out of 10,000 people annually, but likely underdiagnosed (Harney & Patijn, 2007)
More common in people who wear tight clothing, have gained weight, are pregnant, or stand for long periods
Nerve conduction tests may be normal in up to 30% of cases, and imaging rarely shows a clear structural cause
Persistent cases may involve central sensitization, especially when pain persists despite nerve decompression or is more widespread or reactive than expected (Coppieters & Butler, 2008)
Why a Nervous System Approach Helps
In chronic meralgia paresthetica, pain may continue not because of ongoing compression, but due to a sensitized nervous system that keeps interpreting mild input as threatening. This can result in persistent burning, tingling, or fear of movement, even after the nerve has healed. Our approach helps calm the system through pain education, gentle desensitization, sensory retraining, and nervous system regulation, supporting recovery without relying solely on injections, medications, or surgery (Nijs et al., 2014).
-
What it is
Radiculopathy refers to irritation or compression of a spinal nerve root, typically in the neck (cervical) or lower back (lumbar), causing pain, numbness, tingling, or weakness that radiates into the arm or leg. It may result from disc herniation, bone spurs, or narrowing of the spinal canal. In most cases, symptoms improve within a few weeks to months.
Prevalence & Key Stats
Lumbar radiculopathy (sciatica) affects up to 5% of the population, while cervical radiculopathy affects about 0.1% annually (Radhakrishnan et al., 1994; Stafford et al., 2007)
Most cases resolve without surgery, yet up to 30% of patients report persistent symptoms beyond 6–12 months (Yabuki et al., 2012)
MRI findings like disc bulges and nerve compression are also found in many people without symptoms, especially over age 40 (Brinjikji et al., 2015)
Chronic radiculopathy often involves central sensitization, where the brain and spinal cord continue to amplify pain after the nerve has healed (Nijs et al., 2014)
Why a Nervous System Approach Helps
In many chronic radiculopathy cases, pain and sensitivity continue even after the tissue has healed or the nerve is no longer compressed. This is due to a sensitized nervous system, where the brain remains in protection mode and continues to amplify danger signals. Our approach targets this sensitization through pain education, movement retraining, stress regulation, and neurodynamic techniques, helping reduce symptoms, restore function, and build confidence in the body (Coppieters & Butler, 2008; Nijs et al., 2014).
-
What it is
Sciatica refers to pain that radiates along the path of the sciatic nerve, typically from the lower back through the buttock and down the leg. It’s usually caused by irritation or compression of a spinal nerve root (often from a disc bulge), but can also occur without clear structural findings. Symptoms may include sharp, burning pain, numbness, tingling, or leg weakness.
Prevalence & Key Stats
Affects up to 40% of people at some point in their lives (Konstantinou & Dunn, 2008)
Most cases resolve within 6–12 weeks, but up to 30% develop chronic symptoms beyond 3 months (Vroomen et al., 2000)
Disc bulges and nerve compression on MRI are also found in many people without leg pain, especially with aging (Brinjikji et al., 2015)
Chronic sciatica often involves central sensitization, where the nervous system continues to amplify pain signals even after the tissue has healed (Nijs et al., 2014)
Why a Nervous System Approach Helps
When sciatica becomes persistent, the nervous system may be keeping the area in “protection mode” even if the original cause, like a disc bulge has resolved. This can cause ongoing leg pain, hypersensitivity, and fear of movement. Our approach targets the neuroplastic contributors to pain using education, graded movement, desensitization, and nervous system regulation, helping reduce symptoms, improve confidence, and support full recovery without needing injections or surgery (Coppieters & Butler, 2008; Nijs et al., 2014).
-
What it is
A disc bulge occurs when one of the spinal discs, soft cushions between the vertebrae, protrudes slightly beyond its normal space. This is often a normal part of aging and may not cause any symptoms. When a bulge irritates nearby nerves, it can lead to localized back pain or radiating symptoms like sciatica or numbness.
Prevalence & Key Stats
Up to 80% of adults without back pain have disc bulges or other spinal changes visible on MRI (Brinjikji et al., 2015)
Disc bulges are considered a normal age-related finding, not always a cause of pain
Most disc-related back pain improves within weeks to months without surgery or injections (Deyo et al., 1990)
Persistent symptoms may be driven more by nervous system sensitization than ongoing structural compression (Apkarian et al., 2009)
Why a Nervous System Approach Helps
When pain continues after a disc bulge has stabilized or imaging no longer matches symptoms, the nervous system may be stuck in protection mode. This can cause hypersensitivity, muscle guarding, and fear of movement. Our approach helps calm and retrain the nervous system through pain education, graded movement, desensitization, and regulation strategies, empowering you to recover without relying solely on passive treatments or imaging findings (Nijs et al., 2014; Moseley & Butler, 2015).
-
What it is
Spinal stenosis is a condition where the spaces in the spine narrow, potentially putting pressure on the spinal cord or nerve roots. It most commonly affects the lower back (lumbar stenosis) or neck (cervical stenosis) and can cause pain, numbness, tingling, or weakness in the arms or legs, especially during walking or standing for long periods.
Prevalence & Key Stats
Affects up to 11% of older adults, with prevalence increasing significantly after age 60 (Kalichman et al., 2009)
Many people have imaging-confirmed stenosis without symptoms
Pain levels often do not correlate with MRI findings—some with severe narrowing feel fine, while others with mild narrowing report disabling symptoms (Amundsen et al., 2000)
Central sensitization and nervous system hypersensitivity are common in chronic stenosis, particularly when symptoms persist post-surgery or fluctuate with stress (Nijs et al., 2014)
Why a Nervous System Approach Helps
While structural narrowing may be visible on imaging, many people continue to experience pain long after inflammation has subsided or surgery has been performed. This is often due to a sensitized nervous system that continues to interpret movement or posture as dangerous. Our approach helps by calming the nervous system, reducing fear, and retraining protective patterns through education, movement, and regulation strategies, helping patients improve mobility, reduce symptoms, and regain confidence (Apkarian et al., 2009; Nijs et al., 2014).
-
What it is
Patellofemoral Pain is pain around or behind the kneecap, typically worsened by stairs, squatting, running, or prolonged sitting. It is commonly related to how the kneecap moves over the thigh bone during activity, but in persistent cases, the pain is often not due to damage, it reflects changes in how the nervous system processes movement and load.
Prevalence & Key Stats
Affects up to 22% of the general population and is especially common in adolescents, runners, and active adults (Smith et al., 2018)
Up to 91% of people with PFP report chronic symptoms lasting longer than one year (Collins et al., 2013)
Imaging often shows no structural damage, and pain severity is poorly correlated with joint findings (Crossley et al., 2016)
Central sensitization and fear of movement are common in chronic cases, contributing to ongoing pain and disability (Doménech et al., 2014)
Why a Nervous System Approach Helps
In long-standing PFP, the pain often reflects nervous system hypersensitivity rather than injury. The brain and spinal cord may amplify signals from the knee, causing pain during movement that is actually safe. Our approach helps retrain the nervous system using education, graded exposure, desensitization, and nervous system regulation strategies. This not only reduces pain but rebuilds trust in the knee’s ability to move and load again (Nijs et al., 2014; Moseley & Butler, 2015).
-
What it is
Rotator cuff pathology refers to irritation, degeneration, or tearing of the small muscles and tendons that stabilize the shoulder joint. Common symptoms include pain during overhead movements, weakness, and limited range of motion. While some injuries occur suddenly, many develop gradually with no clear cause. In chronic cases, pain often continues even after healing or despite normal imaging.
Prevalence & Key Stats
Partial or full-thickness tears are present in up to 65% of people over age 60, many without pain (Yamamoto et al., 2010)
40–50% of rotator cuff tears are asymptomatic, and pain severity does not correlate with tear size (Minagawa et al., 2013)
After surgery, up to 40% of patients report ongoing pain, even when the tendon is successfully repaired (Galatz et al., 2004)
Central sensitization and fear of movement contribute to persistent shoulder pain in many chronic cases (Dinnes et al., 2003; Lluch et al., 2014)
Why a Nervous System Approach Helps
When shoulder pain lasts beyond expected healing time or imaging doesn’t explain the severity, the nervous system may be amplifying pain signals. This sensitization can cause stiffness, guarding, or fear of using the shoulder, keeping the area in “protection mode.” Our approach focuses on calming the nervous system through education, gentle desensitization, movement retraining, and regulation strategies, helping patients restore strength and confidence, even when previous treatments haven’t worked (Nijs et al., 2014; Moseley & Butler, 2015).
-
What it is
Lateral epicondylalgia is pain on the outside of the elbow, often related to gripping, lifting, or repetitive wrist and forearm movements. While commonly called "tennis elbow," most people who develop it don’t play tennis. The condition is no longer thought to involve significant inflammation. instead, it's often due to sensitivity in the tendon and surrounding nervous system, especially in persistent cases.
Prevalence & Key Stats
Affects 1–3% of the population, especially in people aged 35–54 (Walker-Bone et al., 2012)
Pain typically starts gradually and may persist for over 6 months in up to 20% of cases (Coombes et al., 2009)
Imaging (like ultrasound or MRI) often shows tendon changes in both painful and pain-free elbows, and does not reliably predict pain severity (Connell et al., 2001)
Central sensitization is present in many chronic cases, contributing to pain beyond the local tendon area (Plinsinga et al., 2015)
Why a Nervous System Approach Helps
In chronic lateral epicondylalgia, the pain is often driven more by the nervous system than tissue damage. The brain may continue to interpret gripping or movement as a threat, even if the tendon is strong and structurally sound. Our approach helps reduce this hypersensitivity by retraining the brain and body through education, desensitization, graded loading, and nervous system regulation, helping restore strength, function, and confidence (Nijs et al., 2014; Moseley & Butler, 2015).
Take the First Step to Better Health
Join us on your journey to optimal wellness. Our expert team is ready to provide personalized care and support tailored to your unique needs. Get started today and experience the difference!